Finance leaders in the healthcare sector should be aware that the actual budget for adding to an existing building can far exceed the contractor’s bid once additional costs are added.
Many hospital administrators find themselves contemplating if they should build on campus or retrofit or move physicians into new spaces in response to the many changes in healthcare today, including hospital mergers and expansions, technology implementations, value-based care, and changing patient demographics and needs.
That decision involves many factors, from obvious issues such as cost to more obscure considerations such as hospitals’ and health systems’ reach in their communities. Here are six areas hospital leaders should consider when deciding how to expand their facilities.
Cost
The architect should provide examples of costs for similar facilities so that hospital leaders can consider all costs, not just the price per square foot for construction.
The actual budget for adding to an existing building can far exceed the contractor’s bid once additional costs are added, including permits, new heating and cooling systems to accommodate the extra space, and other costs associated with construction. Hospital leaders should talk with all the experts—the contractor, architect, electrician, lawyer—to determine what other costs are involved and what items might not be part of the bid.
The architect may not be able to provide a standard check list, because every project comes with its own unique challenges, but hospital leaders should expect that the assigned team of architects has experience on similar projects.
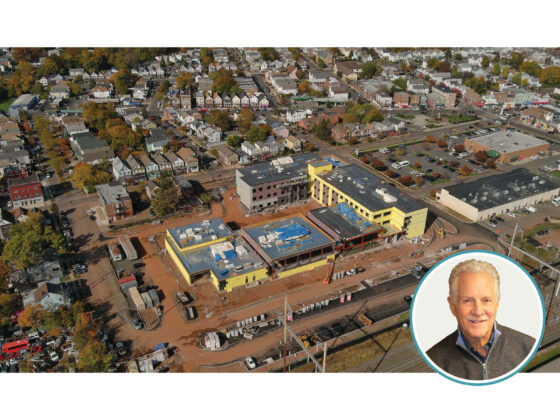
Reach
Many hospitals are feeling the need to compete for patients throughout the state, making reach into other counties a necessity. For example, Hunterdon Healthcare’s main hospital is in Flemington, N.J., Hunterdon County, but hospital leaders were interested in expanding the health system’s services into neighboring Somerset County. They recently opened a renovated 55,000 square foot, three-story building that provides the services of Hunterdon Cardiovascular Associates, Hunterdon Heart and Vascular Center of Bridgewater, Hunterdon Urological Associates, Hunterdon Healthcare Center for Endocrine Health, and Hunterdon Healthcare Physical and Occupational Therapy. The result is convenience for current and new patients who live in Somerset County needing services and treatments closer to home.
Space
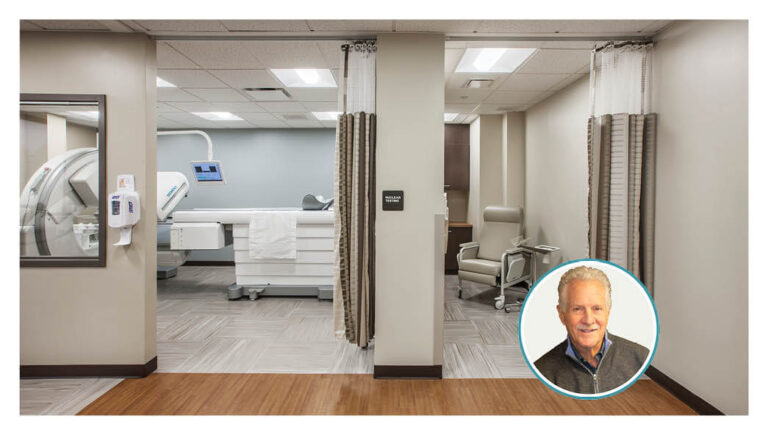
With many procedures that once required overnight stays now being done on an outpatient basis, some hospitals have surplus space that can be repurposed.
One example is St. Peters Hospital in New Brunswick, N.J., which recently refurbished its dialysis lab into admissions, financial advising, and phlebotomy. The relocation and consolidation of these three departments next to the main lobby offers convenience for patients because they typically access those services at the beginning of their hospital stay. In addition, the change allowed for more space and patient privacy, adding to patient satisfaction.
Similarly, new technologies often take up less space, giving hospitals room to reorganize. Even the equipment that was designed around a few years ago has become obsolete. For example, after 15 years, Robert Wood Johnson Health System redesigned a project to accommodate newer, updated technologies.
Interconnectivity of Practices
New construction or retrofit decisions should also include consideration of which practices and administrative services should be together, and which might function more effectively away from the rest of the main building. Placing administrative staff who work directly with patients in the same building as the practices they serve offer convenience and efficiency to patients and staff.
Similarly, providing space for complementary practices, such as housing physical therapy and neurology staff with orthopedists in the same facility, makes it easier for patients to get to their appointments and for physicians to work together to handle patients’ health needs holistically.
Robert Wood Johnson recently redesigned the 3,500 square foot first floor of its Somerset Street medical office building in New Brunswick, N.J., in order to better serve patients by relocating the obstetrics/gynecology and orthopedics offices from the main hospital. Since these services are done on an out-patient basis only, giving them their own space removed the need for patients to find parking and walk through the main building for short visits. The new facility will include a reception and waiting area for patients, five exam rooms, an X-ray room, and physicians’ and staff offices.
Relationship with Community
Because of increasing life spans, more people are in need of geriatric care, bringing medical practitioners and caretakers out of the hospital and office environment and into the communities. Off-campus space can play an important role in a hospital’s commitment to continue to be part of the healthcare team for this demographic.
These spaces are often off-site and can be in different counties and regions, adding new buildings and staff to the budget.
Transportation and Parking
Once a hospital decides that it is time to expand off-campus, location, as with any real estate decision, is the most important feature of a building. The architect and planner are great resources to help hospital leaders find a location that patients — current and new — can get to easily, either on their own or via public transportation.
This article originally appeared in the Healthcare Financial Management Association Strategic Financial Planning newsletter.